15% of medical claims are initially rejected or denied? Yes, this ultimately leads to significant revenue loss and administrative headaches for healthcare providers.
Claim rejections are a major challenge for healthcare organizations because they directly impact the efficiency of patient care. This is why these organizations are turning to healthcare billing solutions that help manage billing processes in a better way.
Let’s explore how medical billing software can help your practice reduce rejections, streamline operations, and, ultimately, improve your bottom line.
An Overview of Medical Billing Software and Claim Rejections

In the healthcare industry, claim rejections occur when an insurance company refuses to process a medical claim due to errors or missing information. Some of the main reasons for rejections include:
- Coding Errors: Incorrect or outdated medical codes that do not match the treatment provided.
- Missing Information: Incomplete patient details or missing documentation.
- Eligibility Issues: Claims submitted for services not covered under the patient’s insurance plan or beyond coverage limits.
Impact of Claim Rejections on Healthcare Providers
A rejected claim can impact healthcare providers in many ways. Let’s look at a few:
- Financial Burden: Rejected claims lead to delayed payments, which can strain a healthcare provider’s cash flow.
- Administrative Overload: Reprocessing rejected claims increases workload, leading to higher administrative costs and reduced efficiency.
- Patient Satisfaction: Frequent claim rejections can also result in billing disputes, negatively impacting patient trust and satisfaction.
Need for Medical Billing Software
Medical billing software has become indispensable in the fight against claim rejections. It mitigates the maximum issues associated with claim rejections. This works by:
- Automating critical tasks
- Detecting coding errors in real-time
- Billing error prevention
- Ensuring compliance with ever-changing regulations
Healthcare IT consulting providers can guide you on selecting and customizing the right medical billing software for your practice. They ensure that all features are fully utilized to reduce claim rejections effectively.
Medical billing software ensures accuracy, reduces errors, and streamlines the submission process. This software not only helps catch errors before they lead to rejections but also enables faster resubmission of corrected claims, thereby minimizing financial loss and administrative hassle.
Organize your billing operations to focus more on patient care.
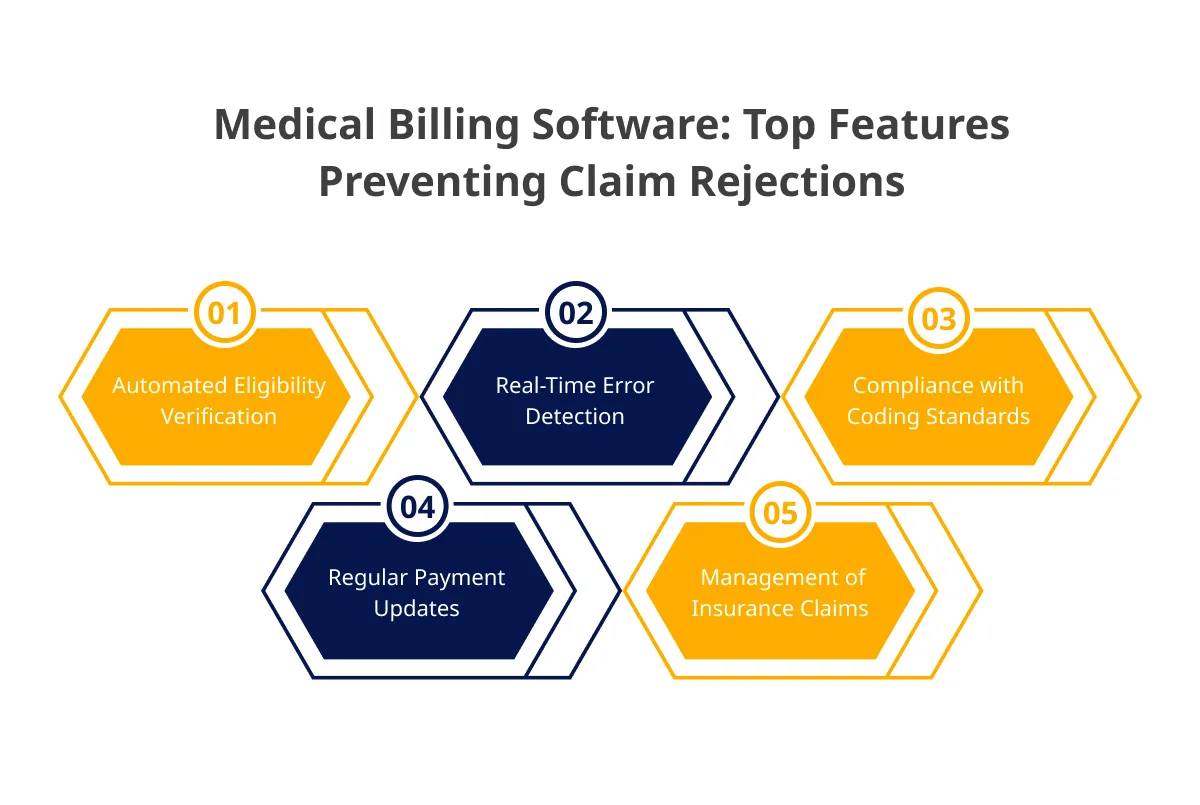
Key Features of Medical Billing Software That Prevent Claim Rejections
The following features collectively help healthcare providers improve their billing processes, reduce errors, and significantly lower the rate of claim rejections. This ensures a more efficient and profitable operation.
1. Automated Eligibility Verification
This feature automatically checks a patient’s insurance eligibility before services are rendered. It verifies whether the patient’s insurance is active, covers the custom healthcare software development services, and ensures there are no discrepancies that could lead to a claim denial.
This feature significantly reduces the chances of claims being rejected due to common problems by catching issues related to ineligibility or expired coverage upfront.
2. Real-Time Error Detection
Medical billing software comes equipped with real-time error detection capabilities that flag potential issues such as coding errors, missing information, or incorrect patient details as you input the data.
This proactive approach allows for immediate corrections, ensuring that claims are accurate and complete before submitting them, thereby reducing the likelihood of rejection.
3. Compliance with Coding Standards
The software is regularly updated to comply with the latest coding standards, such as ICD-10, CPT, and others. It ensures that the correct codes are used for procedures and diagnoses and are aligned with the most current industry standards.
This feature helps avoid rejections due to outdated or incorrect coding, a common reason for claim denials.
4. Regular Payment Updates
This feature facilitates electronic data exchange and provides real-time payment updates, ensuring that your practice stays informed about the status of claims and payments.
By utilizing cloud-based medical billing software that is HIPAA-compliant, practices can maintain secure and efficient payment processes, healthcare data encryption and stay updated on the latest telehealth software developments, minimizing delays and errors.
5. Management of Insurance Claims
Effective claim management software is crucial for the smooth processing of payments in medical practices. Medical billing software automates many time-consuming tasks associated with claims processing, such as tracking claims, handling re-submissions, and detecting fraudulent claims.
This automation accelerates billing tasks, reduces administrative burden, and enhances accuracy, ensuring that claims are processed faster and with fewer errors, ultimately decreasing claim rejections.
Also read: Understanding The Cost Of Building A Custom Medical Billing Software
Healthcare Analytics in Reducing Claim Rejections
Using healthcare data analytics through medical billing software can significantly enhance the accuracy and efficiency of the billing process, reducing claim rejections.
Data Analysis and Reporting
Medical billing software utilizes data analytics to scrutinize past claim rejections, identifying recurring patterns and common issues that lead to denials.
By recognizing these trends, healthcare providers can proactively address potential problems, adjust their billing practices, and implement strategies to prevent similar rejections in the future.
Performance Metrics
The software tracks key performance metrics related to the billing process, such as the time it takes to process claims, the rate of claim denials, and the efficiency of claim submissions.
These insights allow healthcare providers to pinpoint specific areas that need improvement, optimizing the billing process and ultimately increasing the rate of claim acceptance.
How to Streamline the Resubmission Process?
Streamlining the resubmission process using medical billing software can significantly reduce the administrative burden and improve the efficiency of healthcare operations. Here’s how it can be done:
Automated Resubmission
Medical billing software streamlines the resubmission process by automatically identifying errors in rejected claims and facilitating quick corrections. Once the necessary adjustments are made, the software resubmits the claims without manual intervention.
This automation significantly reduces the time and effort needed to correct and resubmit claims, alleviating the administrative burden on healthcare staff and accelerating the payment process.
Tracking and Follow-Up
The software includes robust tracking features that monitor the status of all claims, including rejected ones. It automatically generates alerts and reminders for staff to follow up on pending claims, ensuring no rejected claim is overlooked.
This proactive approach ensures that all rejected claims are addressed promptly, minimizing revenue loss, revenue cycle optimization and improving overall claim management efficiency.
Integration with Other Healthcare Systems
Integrating medical billing software with other healthcare systems is important for ensuring seamless, continuous care for patients. Here’s how to effectively integrate well with existing healthcare infrastructure:
Seamless Integration with EMRs and EHRs
Medical billing software seamlessly integrates with Electronic Medical Records (EMRs) and Electronic Health Records (EHRs), ensuring that patient data is consistently accurate across all systems. This integration allows real-time access to up-to-date medical information, which is crucial for accurate billing and patient data security.
By minimizing data discrepancies between records and billing systems, this integration significantly reduces the likelihood of claim rejections caused by errors in patient information or treatment details.
Coordination Between Billing and Clinical Documentation
Medical billing software effectively aligns billing codes with clinical documentation by cross-referencing the procedures and treatments documented by healthcare providers with the corresponding billing codes. This alignment helps ensure that what is documented in the patient’s records accurately reflects what is billed to the insurance provider.
This coordination reduces the risk of claim rejections by ensuring that the clinical documentation supports the billing codes used, thereby enhancing the accuracy of the claims submitted.
Provide seamless billing process that builds patient trust.
Real-World Success Stories
Have a look at the following case studies that used medical billing software to ensure a fast billing process with no claim denials:
Case Study 1: Reduced Coding Errors
A mid-sized healthcare provider faced a high rate of claim rejections due to inconsistent coding and data entry errors. After using ValueCoders’ robust medical billing software solution, the provider saw a 40% reduction in claim rejections within the first six months.
The real-time error-checking capabilities allowed staff to identify and correct potential issues before submission, leading to a more streamlined billing process and faster approvals.
Case Study 2: Faster Payment Cycles
A large medical group struggled with delayed payments due to the time-consuming process of manually correcting and resubmitting rejected claims.
By adopting our medical billing software with automated resubmission features, the group reduced the resubmission time from weeks to days. This automation expedited the payment cycle and improved cash flow, allowing the practice to operate more efficiently.
Case Study 3: Overcoming Billing Challenges
A small family practice was overwhelmed by the complexities of medical billing, leading to frequent errors and a high rate of claim denials.
Our medical billing software tailored for small practices helped streamline their billing process, reduce errors, and cut down on claim rejections by 30%.
Case Study 4: Enhanced Revenue Cycle Management
A large multi-specialty hospital struggled to manage its complex revenue cycle due to the high volume of patient visits and diverse billing requirements across different specialties.
The hospital implemented our comprehensive medical billing software that integrated with its Electronic Health Records (EHR) system. The software automated the entire billing process, from patient registration to claim submission.
Case Study 5: Patient Payment Management
A mid-sized healthcare provider faced challenges in managing patient payments, leading to delayed collections and increased accounts receivable.
The provider adopted our medical billing software which included robust patient payment management features. This software allowed for easy tracking of patient balances, automated payment reminders, and provided patients with multiple payment options.
Use our billing solutions that enhance accuracy and reduce claim rejections.
Best Practices for Using Medical Billing Software to Reduce Rejections
The following practices show the importance of regularly updating software, training staff, and using continuous monitoring as best practices to optimize medical billing software, ultimately reducing claim rejections.
Regular Software Updates
Keeping medical billing software up-to-date is crucial for ensuring it can handle the latest coding standards, regulations, and payer requirements.
Regular updates help the software comply with industry changes, reducing the likelihood of claim rejections due to outdated or incorrect codes.
Training Staff
Ensuring that all staff members are thoroughly trained in using the medical billing software is essential for minimizing errors.
Proper training helps staff understand how to input data correctly, utilize the software’s features to verify information, and manage claims efficiently, all of which reduce the chances of rejections.
Continuous Monitoring and Improvement
The analytics and reporting features within the medical billing software allow healthcare providers to monitor the billing process continuously.
By analyzing performance metrics and identifying trends in claim rejections, providers can make informed adjustments to improve accuracy and efficiency, leading to fewer denials over time.
Also read: A Complete Guide For Healthcare App Development
Conclusion
Medical billing software changes how healthcare businesses handle claims. It greatly reduces rejections and denials, helping protect financial health. With the right tools, managing the complex world of claims becomes easier and more accurate.
By automating key processes, improving accuracy, and ensuring billing compliance, this technology allows healthcare providers to focus on giving great patient care.
Working with experts like ValueCoders makes this transition smooth. ValueCoders offers healthcare IT solutions tailored to your practice. Embracing medical billing software isn’t just an upgrade—it’s a smart move toward a stronger and more profitable healthcare practice.