Do you know that the global remote patient monitoring market is expected to reach $207.5 billion by 2028? This clearly shows the rapid adoption of RPM technology in healthcare.
While telehealth has revolutionized how we access medical care today, RPM is taking things further by enabling continuous and real-time health data collection beyond mere medical consultations.
This blog post will explain how Remote Patient Monitoring changes personalized treatment plans and why it represents the next frontier in healthcare innovation.
An Overview of RPM & Its Key Components
Remote Patient Monitoring is a healthcare technology that enables continuous monitoring of patient health data outside traditional clinical settings.
RPM provides real-time patient health insights using connected devices and digital platforms, allowing for more proactive and personalized care. Its key components include:
1. Connected Devices
RPM relies on various devices, such as wearable sensors, blood pressure monitors, and glucose meters. These tools collect vital health data, such as heart rate, blood pressure, and blood glucose levels, to manage chronic conditions and monitor overall health.
2. Data Collection and Analysis
The data gathered by these devices is transmitted securely to healthcare providers. Advanced healthcare data analytics tools process this information to identify trends, detect anomalies, and generate actionable insights. This real-time data analysis helps in making informed decisions.
3. Communication Tools
RPM systems include communication platforms that facilitate ongoing dialogue between patients and healthcare providers. These tools allow regular updates, virtual check-ins, and prompt responses, thus creating a seamless connection for better patient outcomes.
Enable 24/7 patient health tracking for faster, more informed medical decisions.
How RPM Personalizes Treatment Plans?
Have a look at the key features of remote patient monitoring technology that enhance personalization treatment plans:
Continuous Remote Monitoring
RPM systems are designed to continuously collect real-time health metrics, such as heart rate, blood pressure, glucose levels, and more.
This constant data stream gives healthcare providers a comprehensive view of a patient’s health over time rather than relying on sporadic in-office visits.
This continuous remote monitoring in healthcare ensures that changes in the patient’s condition are quickly detected, leading to more timely adjustments in care.
Providing Digital Medications
RPM helps patients to take their medicine on time via digital methods or mobile apps. This keeps them on track and reduces the risk of missed doses.
It allows medical providers to identify potential medical adherence problems and intervene when necessary.
For example, if a patient misses his/her dose of medicine, then the RPM alert system reminds the provider to follow up with the patient and address the respective concern.
Detecting Adverse Events
With RPM’s rich and continuous data, healthcare providers can develop and adjust truly personalized treatment plans by identifying any adverse event.
This feature allows healthcare providers to detect adverse events early and prevent harm. Adverse events include infection, an allergic reaction, and any side effects caused by a medicine.
This personalized approach not only improves the effectiveness of the treatment but also enhances patient satisfaction and outcomes.
Use remote monitoring to better manage chronic conditions and improve patient care.
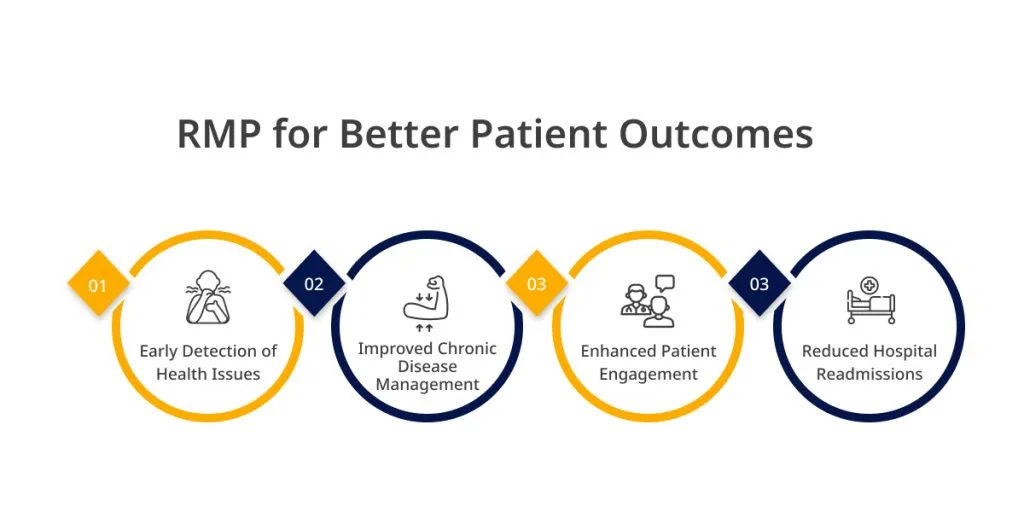
Improving Patient Outcomes through RPM
Remote patient monitoring improves patient outcomes by emphasizing its practical benefits and role in modern healthcare. Let’s see how it works:
Early Detection of Health Issues
Remote Patient Monitoring devices play a critical role in the early detection of health issues by continuously tracking a patient’s vital signs and other health metrics.
RPM for better treatment allows healthcare providers to intervene promptly by identifying potential problems before they escalate into severe conditions.
For example, sudden changes in blood pressure or glucose levels can trigger immediate alerts, enabling timely treatment adjustments and preventing complications.
Improved Chronic Disease Management
For patients with chronic conditions such as diabetes, heart disease, or hypertension, RPM offers significant advantages. Continuous monitoring provides a detailed picture of the patient’s health, allowing for more precise and responsive management of these conditions.
Healthcare providers can adjust medications, recommend lifestyle changes, and monitor the effectiveness of treatments in real time, leading to better long-term health outcomes.
Enhanced Patient Engagement
RPM fosters greater patient engagement by involving individuals more directly in their care. With access to their health data, patients become more aware of their condition and the impact of their daily habits.
This increased awareness encourages proactive behavior, such as adhering to prescribed treatments, making healthier lifestyle choices, and actively participating in their healthcare decisions, all of which contribute to better outcomes.
Reduced Hospital Readmissions
One significant benefit of RPM is its ability to reduce hospital readmissions. By closely monitoring patients after discharge, healthcare providers can quickly identify any signs of deterioration and take necessary action, such as adjusting medications.
This proactive approach improves patient outcomes and alleviates the burden on healthcare systems by reducing the need for costly hospital readmissions.
Read More: – How Medical Imaging Transforms Diagnostics and Patient Care?
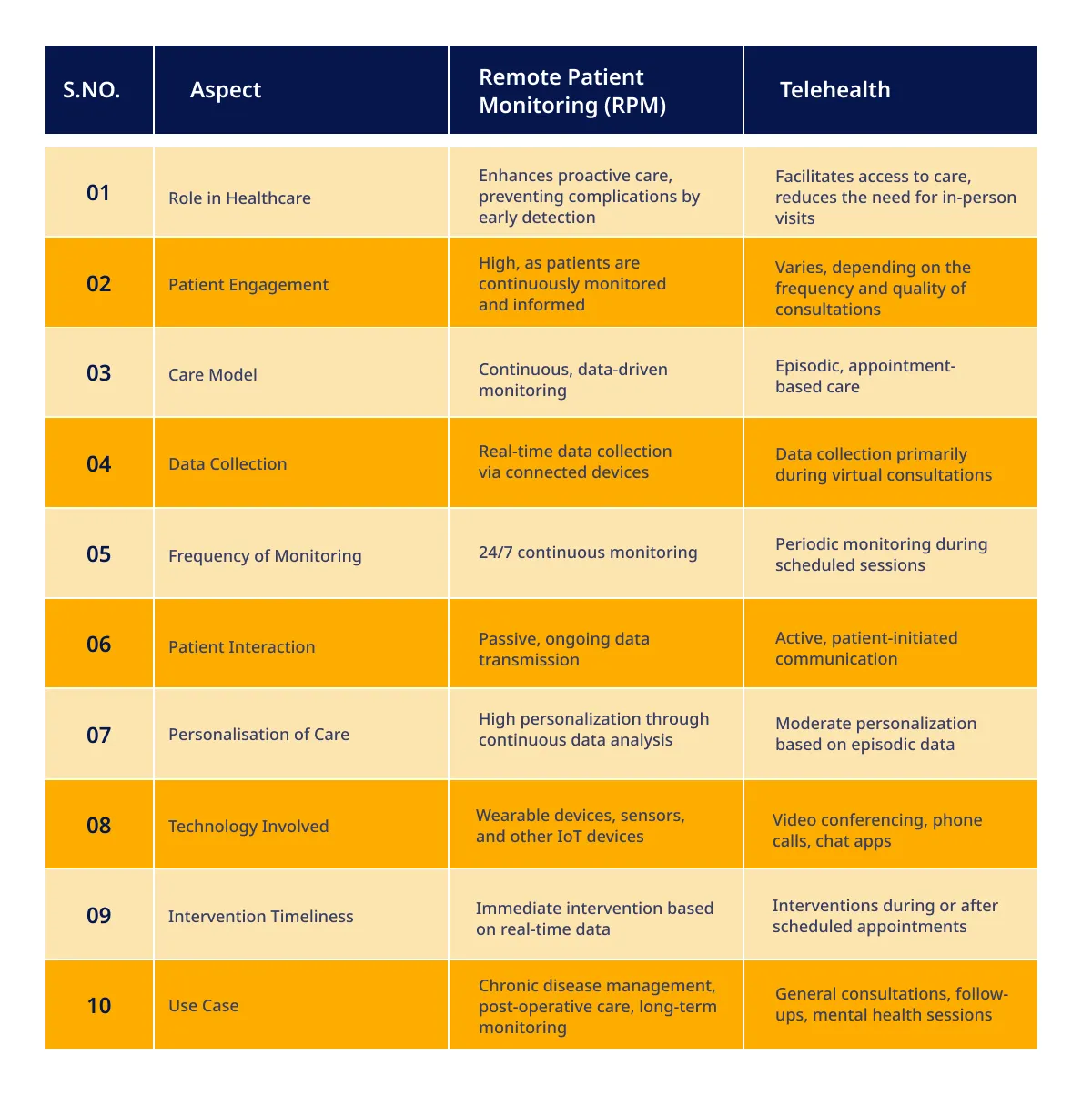
A Comprehensive Comparison of RPM vs. Telehealth
Unlike traditional telehealth, which primarily focuses on virtual doctor-patient interactions, RPM provides a deeper, more personalized approach to managing chronic conditions and improving overall patient outcomes.
While both Remote Patient Monitoring and telehealth are integral to modern healthcare, they operate on fundamentally different principles.
Telehealth provides an episodic care model, where patients consult with healthcare providers during scheduled virtual appointments. This approach is excellent for immediate consultations and follow-ups but is limited to specific points in time.
On the other hand, RPM offers a continuous, data-driven approach. Using connected devices, RPM collects and transmits patient data in real-time, allowing healthcare providers to monitor patients’ health 24/7. This constant data stream enables
- More accurate diagnoses
- Timely interventions
- Personalized treatment plans
Cut hospital readmissions and improve patient outcomes with our remote monitoring solutions.
Comparing RPM with Telehealth
The following table compares RPM and telehealth, showcasing how each serves unique yet complementary roles in modern healthcare. Let me know if you need any further adjustments!
Despite their differences, RPM and telehealth are not mutually exclusive; they serve complementary roles in patient care.
Telehealth provides the platform for direct communication between patients and healthcare providers, facilitating immediate consultation and advice. RPM enhances this by offering the data needed to make informed decisions during these consultations.
Together, they form a more robust healthcare system where telehealth handles communication. RPM ensures the care is based on the most up-to-date and comprehensive data. This synergy ultimately leads to more effective and personalized healthcare solutions, improving outcomes.
Also Read: – How to Build Smart Hospitals? Architecture, Technologies & More
Popular Case Studies of Remote Patient Monitoring
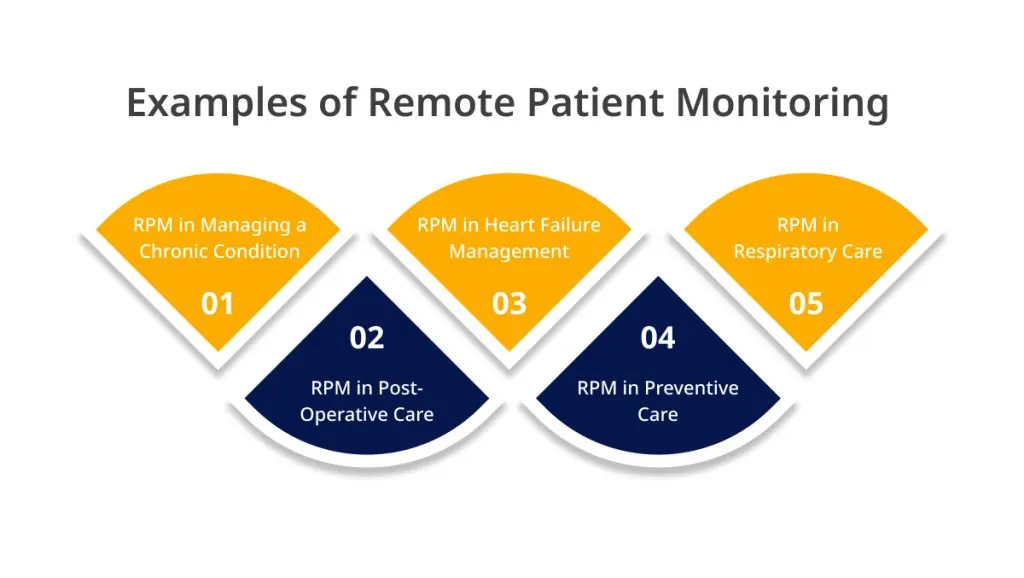
The following case studies illustrate how RPM is utilized in managing chronic conditions and preventing health crises, showcasing its value in improving patient care and outcomes.
1. RPM in Managing a Chronic Condition
In a case of a patient with hypertension, the patient had a blood pressure monitor that transmitted readings directly to their healthcare provider. This continuous data flow allowed the provider to detect a pattern of elevated readings during specific times of the day.
As a result, the treatment plan was adjusted to include medication at those critical times, leading to better blood pressure control and reducing the risk of complications.
2. RPM in Post-Operative Care
A surgical patient recovering from heart surgery was monitored using RPM to track vital signs such as heart rate, oxygen levels, and blood pressure. Through continuous monitoring, the healthcare team detected a slight but consistent decrease in oxygen saturation levels.
Hence, Prompt intervention included adjusting the patient’s oxygen therapy, preventing a potential post-operative complication, and ensuring a smoother recovery process.
3. RPM in Preventive Care
RPM is utilized for monitoring at-risk populations, such as elderly individuals with cardiovascular conditions. The system alerts providers to any significant changes that could indicate a potential health issue before it becomes critical.
Early detection of potential health issues leads to preventive interventions and reduces the risk of severe conditions. Patients also receive timely advice and treatment, improving overall health and reducing emergencies.
4. RPM in Heart Failure Management
Patients with CHF have weight scales, blood pressure cuffs, and wearable devices that monitor heart rate and oxygen levels. Sudden weight gain, a common sign of fluid retention, triggers alerts for immediate medical intervention.
This approach reduces hospital readmissions, improves patient outcomes, and enhances the quality of life by preventing severe complications.
5. RPM in Respiratory Care
If a patient’s lung function deteriorates or oxygen levels drop, the healthcare team can intervene with treatment adjustments or recommend hospitalization if necessary.
Improved management of COPD, with fewer exacerbations and hospitalizations. Patients experience better control of their symptoms, enhancing daily functioning and reducing healthcare costs.
Use RPM to monitor progress and refine care for better, long-lasting health results.
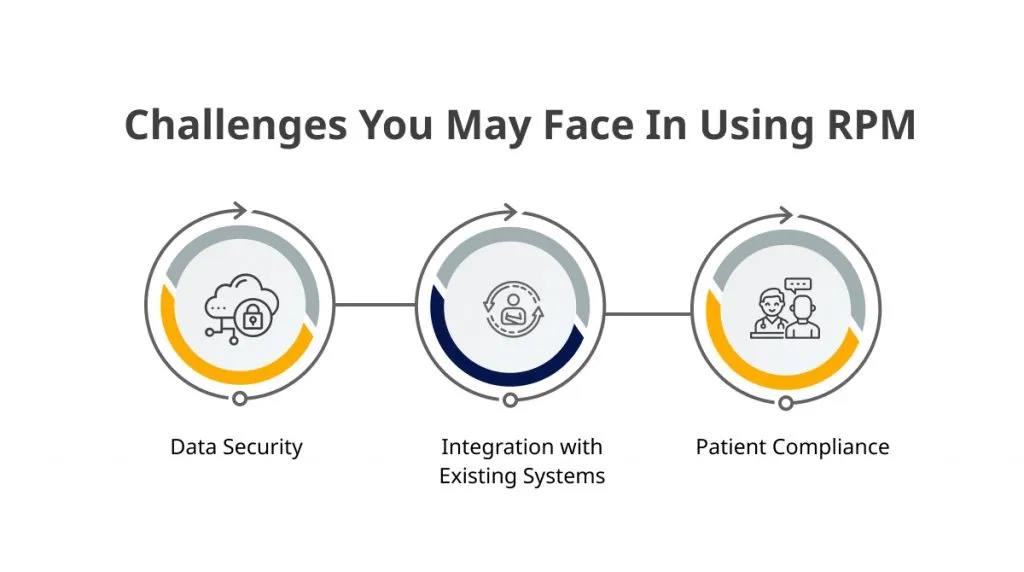
Challenges & Solutions for Using RPM
The following key challenges of remote patient monitoring present insights into how they can be managed to ensure the successful implementation of RPM in telehealth services.
Data Security
Continuous data collection from various devices transmits and stores a significant amount of sensitive information. Healthcare providers must do the following things to protect this data:
- Implement robust encryption protocols
- Secure communication channels
- Strict access controls
- Compliance with regulations like HIPAA
Also Read: – ChatGPT in Healthcare: Opportunities and Challenges in Patient Interaction
Integration with Existing Systems
Many healthcare providers already use a range of electronic health records (EHRs) and other digital tools to ensure that remote patient monitoring data seamlessly integrates with these systems but this can be complex.
Since, poor digital health and RPM integration can lead to data silos, inconsistencies, and inefficiencies that undermine the effectiveness of RPM. This requires:
- Careful planning
- Selection of compatible technologies
- Custom healthcare software development
Patient Compliance
The success of RPM heavily depends on patient compliance. Hence, patients must consistently use the monitoring devices and adhere to the protocols set by their healthcare providers.
However, ensuring compliance can be challenging, especially if patients find the technology difficult to use or perceive as intrusive. To improve compliance, it is important to
- Choose user-friendly devices
- Provide adequate training
- Offer regular support
- Foster a robust patient-provider relationship
Future of RPM & Personalized Healthcare
RPM empowers healthcare providers to make informed decisions tailored to each patient’s unique needs. This not only enhances the effectiveness of treatment plans but also fosters more robust patient engagement.
Have a look at the technological advancements in RPM and the broader impact on healthcare accessibility for long-term outcomes.
- AI, Machine Learning, and Predictive Analytics will provide more accurate and timely health predictions. AI/ML for healthcare enhances RPM’s ability to provide personalized insights, allowing for proactive interventions and more tailored treatment plans.
- RPM will extend healthcare services to underserved populations, including rural areas with limited access to healthcare. By reducing the need for in-person visits, RPM helps bridge the gap in healthcare disparities, ensuring that more people receive quality care.
Healthcare providers benefit from more efficient resource use, reduced hospital readmissions, and the ability to deliver more proactive and preventive care, ultimately leading to cost savings and improved patient satisfaction.
Conclusion
Remote Patient Monitoring stands out as a game-changer in the healthcare sector. It is moving beyond the limitations of telehealth to offer truly personalized care.
Integrating RPM into everyday healthcare practices promises to revolutionize patient outcomes, making personalized, data-driven care the new standard. Let’s connect with our healthcare IT consulting experts at ValueCoders to get your next project done using RPM.
We are one of the top healthcare software development companies in India since 2004. We have successfully delivered 4200+ projects worldwide. Contact us today!